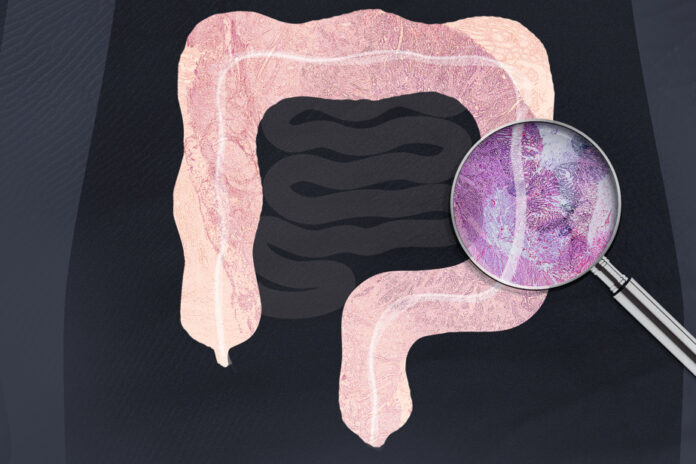
The latest Canadian and American data confirm it: younger and younger populations are increasingly at risk of developing colorectal cancer. And doctors are looking for explanations.
It is a story that repeats itself.
The story of men and women often in great shape, who have not yet reached their mid-fifties. The history of symptoms that appear. Some abdominal cramps. Weight loss. Blood in the stool.
At that age, it’s nothing serious, they say. Maybe stress or hemorrhoids.
But the months pass and the symptoms persist. A colonoscopy is required.
Then, the verdict falls, like a cold shower: colorectal cancer, advanced stage.
This story, Catherine Dubé has seen and reviewed it in recent years. The gastroenterologist is the clinical lead for Ontario’s colorectal screening program.
“It’s always a big shock to see such young cancer patients,” she insists. These diagnoses are remembered all our lives. »
The shock has been more and more frequent in recent decades. Diagnoses of early colorectal cancers are rising rapidly in many parts of the world. According to a recent report by the American Cancer Society (ACS), the number of cases among people under the age of 55 has been increasing by 1-2% each year in the United States since 1995.
In Canada, the annual increase in different types of colorectal cancer among 20 to 49 year olds varied between 1 and 4% from 2000 to 2017, according to the latest data published in The American Journal of Gastroenterology (these calculations exclude Quebec, for lack of of data). Same story in most industrialized countries.
How to explain this phenomenon ? The question is on everyone’s lips among gastroenterologists.
In Canada, colorectal cancer is the third most common cancer, according to the Canadian Cancer Society.
Older people remain significantly more at risk, notes the ACS in its report. Each year, among those 65 and older, 161 out of 100,000 people are diagnosed, compared to 69 out of 100,000 people aged 50 to 64 and 12 out of 100,000 people aged 20 to 49.
However, the increase in cases among the youngest coincides with a decrease observed among the oldest, in particular due to the best preventive measures.
“There is an increased risk for people born after the 1950s, which is called a cohort effect,” says Rebecca Siegel, scientific director of the ACS and co-author of the report. “We are trying to understand the changes in the products that people have been exposed to over the years. »
“It must also be said that this type of cancer takes 10 to 15 years to develop,” adds the scientist. So when you see 30-year-olds being diagnosed, that means they were exposed [to risk factors] early in life. »
Unraveling the mystery of early colorectal cancer will be a daunting challenge, notes Manuela Santos, professor in the department of medicine at the Université de Montréal. “You would have to follow a really large population and monitor, for example, diet and exposure to environmental factors over a long period of time to see if, 10 years later, people are developing cancer. It is difficult and expensive. »
To provide some possible explanations, the researcher, affiliated with the Montreal Cancer Institute, relies on the study of the intestinal microbiota. This set of microorganisms has been particularly affected by the growing consumption of antibiotics among young people in recent decades.
Changes in eating habits have also caused transformations in the microbiota. The consumption of sugary drinks or processed products, for example, are risk factors for colorectal cancer, according to several studies.
Also in the dock are environmental toxins, which can damage the colon.
Cases of colorectal cancer in young people are not only more frequent. They are also diagnosed at later stages, according to data from the ACS.
A study published in 2017 by researchers at Stanford University, California, also reveals that in people under 50, the diagnosis falls on average 40% later than in older people.
“Young people usually wait longer before seeing a doctor,” says Rebecca Siegel. And even doctors often think it’s nothing major, given their age. »
When the disease is detected early, the survival rate increases dramatically, from 12% when diagnosed at stage 4 to 92% when diagnosed at stage 1, according to the Canadian Cancer Society. A lesion can also be discovered and removed even before it turns into a tumour.
Several countries have therefore set their sights on screening in an attempt to offset the increase in cases. In 2021, the United States lowered the age for the start of screening to 45 years old, rather than 50 years old.
In Quebec, a motion passed in the National Assembly in early April urges the government to roll out a systematic screening program. The province is the only one in Canada that does not have this type of program.
The association of gastroenterologists of Quebec has been requesting it for several years now, without success. Another story repeating itself.