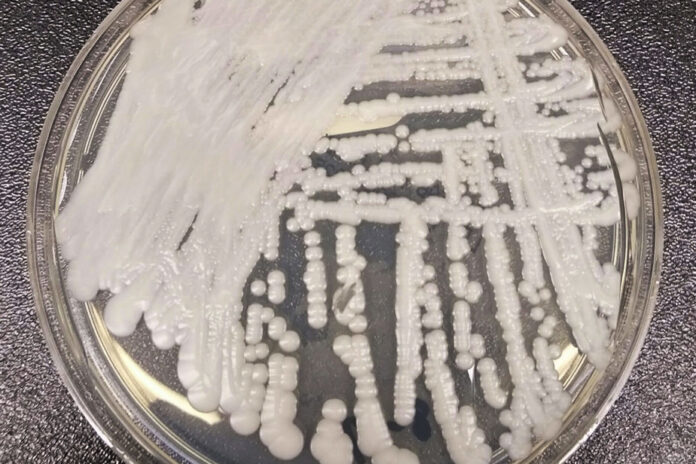
The Candida auris fungus, which primarily attacks hospitalized people, has spread “at an alarming rate in US healthcare settings in 2020-2021”, according to a new report from the Centers for Disease Control and Prevention (CDC) released Monday.
The number of cases in the United States has increased from 476 in 2019 to 1,471 in 2021. “And it’s still going up. The figures we have so far from 2022 [in the United States] are much worse than those from 2021. This is certainly very concerning,” said Simon Dufresne, microbiologist at Maisonneuve-Rosemont Hospital.
The number of cases detected in Canada is much lower. Since 2012, 43 cases of Candida auris have been reported to the Public Health Agency of Canada, including 35 in the past five years. Among these cases, 19 come from Quebec and Ontario, including two patients who were infected with the fungus at the Pierre-Boucher hospital in Longueuil last September.
But it’s only a “matter of time” before we see an increase in its presence in Canada, says Adnane Sellam, researcher at the Montreal Heart Institute and Candida auris specialist. “You have to expect [to observe an increase] and you have to prepare for it,” adds Mr. Dufresne.
The mortality rate is around 30 to 60%, but this proportion must however be qualified. Indeed, one can be colonized by the fungus without developing a real infection, says Sellam. This “super resistant” yeast can lodge on the skin without causing symptoms.
Some patients, often those with weaker health or weakened immune systems, will however develop the infection. In these cases, the yeast enters the bloodstream and spreads throughout the body, says Sellam. It then causes symptoms such as fever and chills.
Infection with this fungus mainly affects hospitalized or immunosuppressed patients. It is transmitted by direct contact or by surfaces, but not by aerosols. Patients who have been hospitalized in a healthcare facility for a long time, who have a central venous catheter, or who have previously received antibiotics or antifungal medications appear to be most at risk of infection with this yeast, details the CDC. .
Infection with this fungus is often resistant to several drugs commonly used to treat it. “We don’t have a lot of [treatment] options. This is a huge cause for concern because a physician or infectious disease specialist should always have options to treat these patients,” Sellam says.
In the United States, the number of cases resistant to echinocandin, the most recommended antifungal drug for the treatment of this infection, tripled in 2021. In Canada, one-third of cases were multidrug-resistant.
We need to be prepared to screen patients for this organism, says Dufresne. “Since 2017, we have had protocols in Quebec as much to guide hospitals if we have a colonized or infected patient as practice guides for laboratories,” he explains. “Since there are few cases in Canada, it’s probably a bit early to launch a very aggressive surveillance program, but we are on high alert,” he adds.
Possibly. According to Canada’s National Collaborating Center for Infectious Diseases, there is reason to believe that rising temperatures due to climate change are contributing to the spread of the fungus. “As soon as there is an increase in stress, in this case heat, [the fungus] can mutate, predisposing it to be a human pathogen,” says Sellam.